An Intimate Pandemic: The Community Impact of Influenza in 1919
In the final year of World War I, an extraordinary disease emerged – the pandemic of pneumonic influenza or ‘Spanish flu’. Highly infectious, it affected military and civilian populations equally, soon reaching almost all parts of the globe by the Armistice of November 1918. The immediacy of the crisis – its fear, suffering and mourning – remained intense in the memories of many who lived through it.
Because pneumonic influenza targeted adults in the prime of life, it cut across the workforce and a generation of parents. Its impact was therefore felt in almost every community and family around the globe. As a result, it is likely to be a part of nearly everybody’s family history and local history. In this sense, it truly was an intimate pandemic.
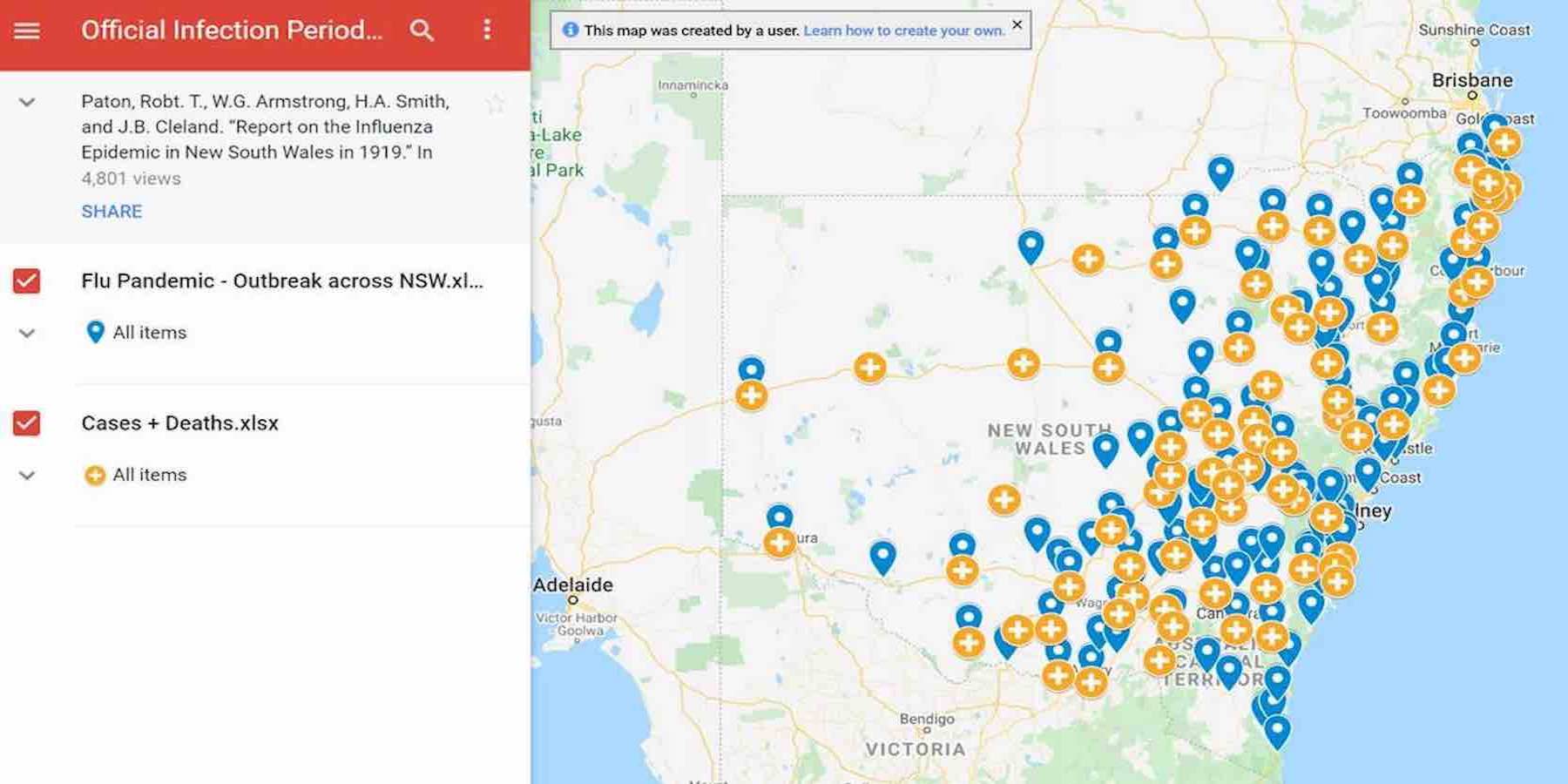
This website offers an overview of pneumonic influenza in Australia, especially its effect upon communities throughout New South Wales. It complements the RAHS research guide as a source of information and inspiration to begin your own investigation into its local or family impact. We urge community historians to share their research through publications, websites, presentations, media stories or commemorations. If you do create a ‘Spanish flu’ project, we’d love to hear about it.
Your Title Goes Here
An Unstoppable Enemy
The pneumonic influenza crisis of 1918–19 was a medical catastrophe on a scale unequalled since the ‘black death’ of the middle ages. It is estimated to have infected approximately a quarter of the world’s population, killing between fifty and 100 million people. [1] While the true toll will never be known, in the space of two years this astonishing disease caused at least three times as many deaths as the four years of fighting through World War I.
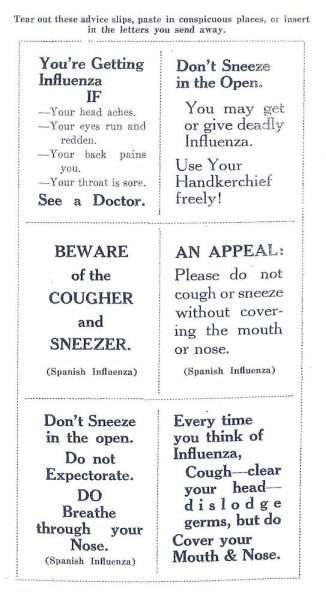
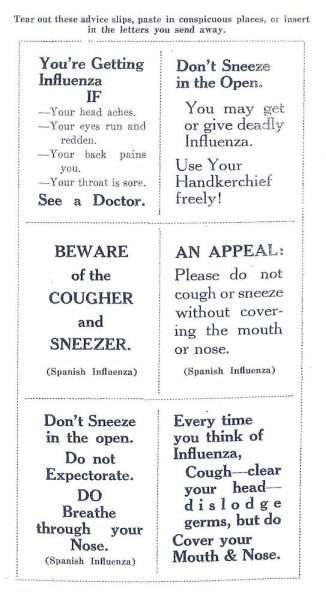
Excerpt from Wade Oliver, ‘Spanish Influenza: All About It’, (Melbourne: Speciality Press, 1919), p. 24.
The result was that a serious infection soon became a particularly deadly one, quite different in character from the seasonal influenza that occurred each winter. It came to be known as the ‘Spanish’ influenza not because it began in Spain, but because that country was neutral during the war and its newspapers did not censor accounts of the new disease ravaging armies and civilian populations alike. [3] Most alarmingly, pneumonic influenza was up to 25 times deadlier than typical influenza epidemics. [4]
An Explosive Spread
Although one of history’s most lethal diseases, much still remains unknown about the pneumonic influenza of 1918–19. At the time, however, its medical and social impact were well documented. The flu was very easy to catch, particularly after sharing enclosed spaces such as public transport, small offices or bedrooms. Nevertheless, it could also be contracted in larger public gatherings such as church services or agricultural shows. Victory celebrations were notorious for sparking an explosive spread of the flu into local communities. [5]
Individual responses to infection varied a great deal, and many people suffered only mild forms that resembled a bad cold or seasonal influenza. For those who developed a more serious case, typical signs and symptoms included a rapid onset of sneezing, sore throat, coughing, difficulty breathing, headache, tiredness, chills and a fever. Early bed rest might help the sufferer recover within one to two weeks. However, trying to stay active was a common reason for the infection worsening, and possibly turning fatal. [6]
By mid-1918 the pandemic had earned a terrifying reputation for its high mortality. It was usually known at the time as ‘pneumonic influenza’ because this new strain of disease frequently led to deep-seated chest infections. Many deaths caused by the flu were indeed classified as ‘pneumonia’ as victims effectively suffocated when their lungs filled with fluid. Others died from heart failure or exhaustion. [7]
The severe stage was accompanied by difficulty breathing and even delirium (moving in and out of coherent thought and behaviour). It was characterised by a typical rosy flush in the cheeks, which then turned mahogany, plum-coloured or blue. Doctors found that the bluer the patient’s face, the worse their outlook. [8] Victims who died usually did so in the first week, while those who survived this life-threatening form regularly took three to four weeks to fully recover.
The Tide of Infection

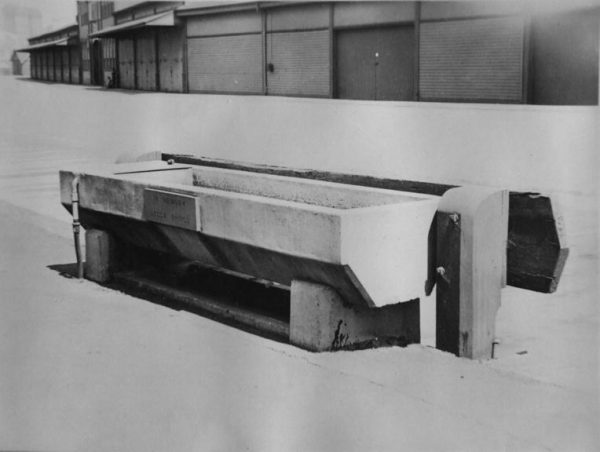
Fumigation chamber on SS Port Darwin 1919 [Image courtesy Australian War Memorial, J02824]
This was the largest mass movement of people into the continent since the gold rushes of the 1850s, and many of these ships carried influenza cases aboard. By October 1918 the first vessels bearing ‘Spanish’ flu cases had reached Australian quarantine stations, where 2,795 patients were detained, hundreds of them eventually dying. [2] Although it seemed that the quarantine border might hold, advice from around the world warned Australian governments and community groups to prepare for an unprecedented breakdown of social services.
An emergency meeting of Commonwealth and State Governments was held in November 1918, and a series of centralised emergency measures agreed to. [3] Unfortunately this accord broke down almost immediately after pneumonic influenza was found to have come ashore in January 1919. As a result, throughout the crisis the Commonwealth Government largely remained responsible for maritime quarantine and immunisation, while individual states managed their own precautions and regulations. [4]
Cutting through the Community

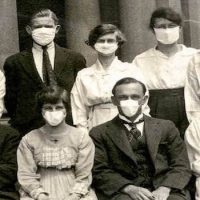
Female typists in masks 1919 [Image courtesy State Library of NSW, 00508]
One result was that the infection cut through the community, incapacitating civic leaders, health professionals and essential workers at the moment they were needed most. Furthermore, a significant proportion of Australia’s nurses and doctors remained overseas through the early months of 1919, awaiting repatriation. These were precisely the practitioners most familiar with the disease and how best to manage it.
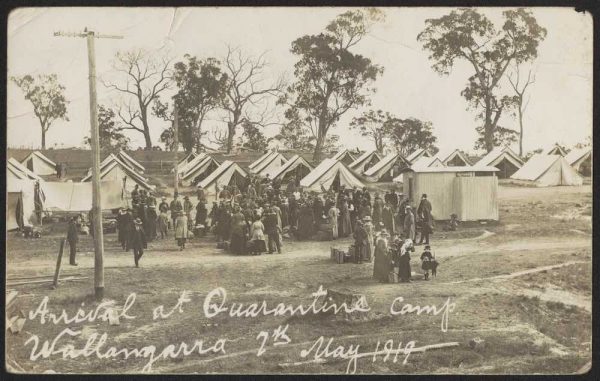
Although the clinical features of pneumonic influenza were soon understood and feared, doctors and scientists could offer little to thwart or treat this deadly infection. Medical advice focused on preventing the flu from spreading, including wearing gauze or muslin face masks, regularly washing hands, gargling spirits, cleansing the nasal passages with salty liquid, or inhaling steam infused with zinc sulphate, a chemical believed to help kill the flu ‘germ’. [6]
Limited Treatment or Prevention Options
Excerpt from Wade Oliver, ‘Spanish Influenza: All About It’, (Melbourne: Speciality Press, 1919), p. 21.
Treatment for diagnosed cases could include paracetamol or aspirin to reduce pain and fever, but it did not target the underlying infection – effective antibiotics were still decades away. The pandemic also prompted brisk sales of patent ‘remedies’ of dubious value. Ultimately, the best advice that could be offered to patients was rest, nutrition and nursing care.
In 1918–19 it was not known whether influenza was caused by bacteria – ‘germs’ – or by much smaller viruses, which could not be detected by the microscopes then in use. Based on bacterial samples, the Commonwealth Serum Laboratories in Melbourne produced three million doses of an immunising ‘flu vaccine’ for use around the country, but its value was never properly tested. [7]
In New South Wales, the Department of Public Health also manufactured a similar vaccine, which was administered to nearly a quarter of the state’s population. While it did not necessarily prevent infection, vaccinated residents who caught pneumonic influenza appeared to suffer a milder, less fatal form of the disease. [8]
Influenza Comes Ashore
The deadliest version of the flu circulated in the final months of 1918, just as the war was ending. As it continued spreading across the globe through 1919, the infection took on milder characteristics. This was the disease that reached Australia’s coastal quarantine stations in October 1918 and came ashore in January 1919.
By that time many Australians had already suffered or observed the disease while serving overseas with the Australian Imperial Force, or in naval, nursing or medical units. Many more encountered the flu on the troopships that brought them back home across the Indian and Pacific Oceans. [1]

Soldiers at Randwick Military Hospital 1914–18 [Image courtesy Randwick Library, M00030]
Few Towns or Cities Escape
Early in January 1919, the pandemic came ashore in Victoria. On 22 January the first case – a soldier – arrived by train in Sydney. He was treated at Randwick Military Hospital, but his illness was not at first diagnosed. By the time it was realised that ‘Spanish flu’ was in Sydney, the infection had spread to staff and visitors, and hence into the community. Trains, roads and coastal shipping all helped distribute the disease across the state. Few cities or towns escaped, although some were much harder hit than others. [4]
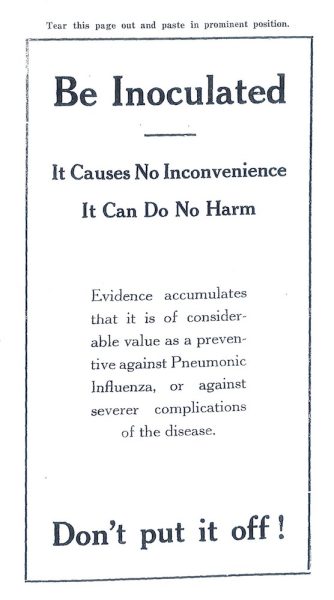
Because of political disagreements between the states, many closed their borders with each other. New South Wales quarantined itself from Victoria on 30 January, followed by South Australia and Queensland. As a result, hundreds of New South Wales residents were stranded away from home, especially along the Murray River and the Queensland border. [5]
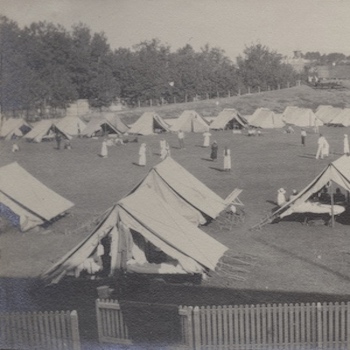
Concurrently, border towns such as Albury and Tenterfield were faced with managing hundreds of potentially infected Victorians and Queenslanders trapped in New South Wales. These individuals and families had to fall upon the charity of locals while pleading for government support. Finally a series of quarantine camps was set up at major crossing points, but the borders were easily breached by travellers desperate to return home. [6]
A Critical Benefit of Quarantine
Arrival at quarantine camp Wallangara, 7 May 1919 [Image courtesy State Library of Victoria, H2016.356_1]
As a result, the overall death toll across the nation was approximately 15,000 people. [8] At about 0.2% of the population, this rate was one-tenth that in New Zealand. In Western Australia and Tasmania, which were infected later in 1919, mortality was much lower again. Regional differences also counted: the death rate in regional and rural Australia was about 55% lower than in metropolitan areas. [9]
Although Australia’s death toll was small by global standards, it came on top of the nation’s 62,300 war dead. In fact, with ‘Spanish flu’ killing 15,000 Australians in less than a year, its morbid impact was approximately the same as the annual death rate for the Australian Imperial Force over 1914–18. [10]
Into Homes and Hearts
Over the course of January to September 1919, pneumonic influenza infected approximately a third of the entire population of New South Wales. Reaching many country communities over March to July 1919, its explosive local impact saw ‘Spanish flu’ matched by an epidemic of fear. [1] Families, businesses, congregations and social groups had to decide whether to isolate themselves or actively address the escalating crisis.
Nowra Public School converted into a temporary hospital for pneumonic influenza epidemic, 1919 [Image courtesy Sydney Living Museums, 41328]
Communities responded in quite different ways. [5] ‘The country districts round Nowra’, reported local doctor Frederick Rodway, were ‘not invaded to any great extent, as the country people practically quarantined the town’. [6] The opposite was true at Alstonville, mid-way between Ballina and Lismore. The local council ‘demanded a certificate of health from persons seeking to enter the Shire’, remarked Dr Roy Graham. [7] Unfortunately they relented to allow returned soldier Percy Latimer to marry local girl Ilene Bell on 28 May. Coughing through the 1½ hour ceremony in Alstonville’s small Presbyterian Church, Percy was so ill upon reaching Ballina that he spent his honeymoon in the local hospital. Within three days, twenty of the twenty-three people who attended the wedding had come down with pneumonic influenza. [8]
The Silent Tragedy of Expectant Mothers

Nurses leaving Blackfriars Depot Chippendale, April 1919 [Image courtesy State Archives & Records NSW, NRS4481_St6674]
This difference was probably not biological, but behavioural. Men were more likely to press on in the face of early symptoms, meaning that their cases became more serious before they collapsed. Even health experts ignored their own advice, including Charles Savill Willis, Principal Medical Officer of the Department of Education.‘ So keen was Dr. Willis’ sense of duty at the commencement of his brief illness’, noted the preface to his posthumously published book on sanitation, that ‘he actually delivered an address to the Dental Association of New South Wales’. [11]
An often silent tragedy also unfolded among expectant mothers. Pregnant women died at the appallingly high rate of 26.7%, and just about every pregnancy that was not at full term resulted in a miscarriage or stillbirth. Babies delivered alive were also at high risk: nearly 30% of them also died if their mother was infected. [12]
Death rates varied enormously between communities and localities. Central and inner Sydney were hard hit, as was Newcastle and the Hunter region, alongside industrial and mining towns such as Lithgow and Broken Hill. [13] The impact upon Indigenous residents of New South Wales is particularly poorly documented, and warrants detailed local history research.
In 1919, only Queensland maintained disease and death registers for Aboriginal people. These documents suggest that the Indigenous death rate from pneumonic influenza was 10–20 times higher than in the general population. [14] Many who came down with the illness were locked into disease compounds, with few facilities or even basic shelter. Furthermore, notes Indigenous scholar Gordon Briscoe, ‘Aborigines acted in a customary way when threats to their belief system surfaced. Many inmates of these disease-compounds reacted quickly by escaping for refuge in the bush as the number of deaths from influenza rose’. [15] These Queensland observations match a 1919 report from the Casino-Lismore area, by local doctor Roy Graham. Among the 110 inhabitants of the Aboriginal ‘compound’ at Stony Creek, near Kyogle, there were 62 cases and 12 deaths from pneumonic influenza. [16] This death rate of 10.9% was 24 times higher than the New South Wales average. Furthermore, Graham noted, the first deaths ‘so scared the remaining people in the Hospital … that they made their escape during the night’. [17] The tragic result was that the infection was transferred to nearby communities, while other Indigenous victims walked as far as Coraki to the south and Fingal to the north, carrying pneumonic influenza with them.
Regulation and Mobilisation
From late January 1919, the New South Wales Government introduced the nation’s most severe and far-reaching regulations. Its responsibilities were coordinated by a Metropolitan Influenza Administrative Committee – later renamed the Influenza Emergency Committee – which worked in conjunction with the Country Influenza Administrative Board.
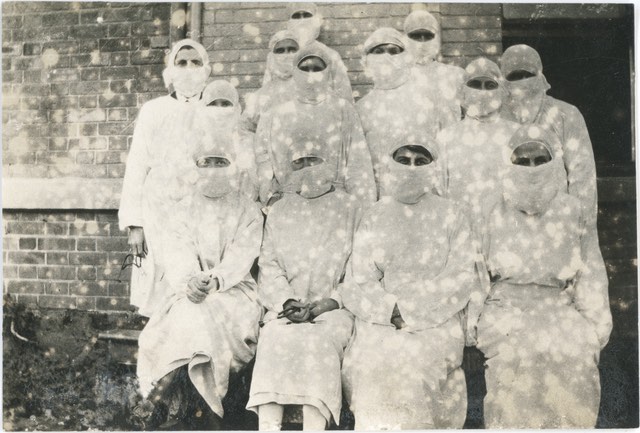
Group of nurses wearing masks, Photographer unknown, 1919 [Image courtesy of the Macleay Museum, University of Sydney, HP85.8.87]
The requirement that residents wear gauze or muslin face masks while on public transport or in enclosed spaces further contributed to the climate of fear. Additional preventive measures also became widespread, including immunisation depots and public inhalation chambers to cleanse the airways. [2]
Despite this overall coordination at state level, municipal and shire councils were significant providers of health, sanitation and welfare services in 1919. [3] As such they bore the brunt of the influenza pandemic, as well as the civic consequences of their decisions.
Some municipal authorities and affected organisations protested against the government’s regulations, while others mobilised to coordinate a collective response. [4] ‘My Club decided to abandon their meetings’, noted Harold McLean, the honorary secretary of the Cowra Pony Race Club, on 11 February. [5] Conversely, on 19 April the secretary of the local Health Committee requested ‘that the restrictions imposed upon Braidwood by [the NSW Government] Gazette should be withheld’. [6] ‘If it is the wish of the Mayor and Administrative Committee to remove the restrictions’, came the Minister for Public Health’s reply, ‘it will be done’. [7]
Volunteers Step into the Front Line
In many areas, the disease itself steamrolled over the best-laid plans. Because pneumonic influenza rapidly infected up to a third of residents, it often overwhelmed local services and emergency preparations. Fear of the flu, falling sick with it or nursing affected family members further limited the numbers of those able to assist. In communities such as Cooma, commerce, social services and medical care crumbled in the wake of so much illness and debility. [8]

Influenza emergency worker, metal badge, made by Angus & Coote Ltd, Sydney, 1919. Donated by Miss Annie Hodge 1946 [RAHS Manuscript Collection]
Reminiscent of the voluntary spirit of the war years, these acts of courage and compassion by local men and women deserve recognition and commemoration. Volunteers often stepped into the front line, exposing themselves to the risk of contracting the deadly infection. Sadly, many succumbed.
For instance, a headstone at Marlee General Cemetery, near Port Macquarie, records the death of Marion Robertson on 12 July 1919. A nurse who had resigned to marry, she volunteered to return to duty at the emergency hospital in Wingham. In nursing patients with pneumonic influenza, Marion contracted a fatal dose herself. [10] Tragically, her headstone also records the death of her brother, Bombardier Raymond Robinson. He had also died from ‘Spanish flu’ in a military hospital in England just two days after the Armistice in 1918. The family’s double blow of grief reminds us that this was indeed an intimate pandemic.
Grief, Recovery and Memory

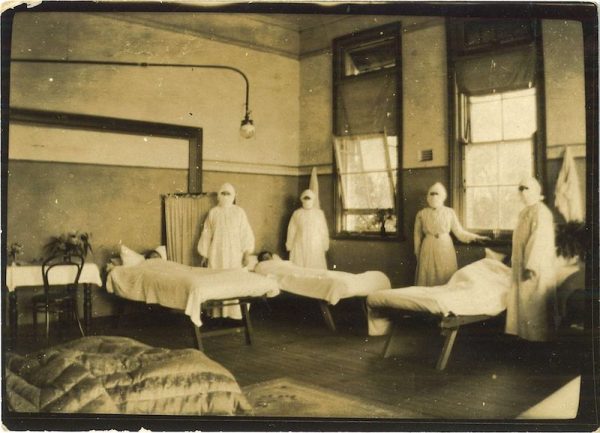
Jack Kaines – Crowd at Quarantine Camp [Image courtesy State Library of South Australia, PRG] 1638_2_55]
Taking away both breadwinners and unborn babies, the pandemic deeply tested faith, whether in modern medicine or a higher being. Yet it also illustrated the potential for communities – local women and men – to rise to an unprecedented challenge and serve the common good. For this reason, if no other, the intimate pandemic of pneumonic influenza merits reflection, research and commemoration. [2]
After the emergency was declared over in September 1919, individuals, families and communities recovered and focused on building a post-war world. Unlike the numerous memorials to the Anzacs who served and died over 1914–18, however, there are relatively few monuments to the victims and volunteers of 1919. [3] Was the pandemic forgotten? [4]
Not entirely. A large memorial in central Bathurst commemorates local doctor John Brooke Moore, who bore an enormous burden of care through the pandemic crisis. [5] At Waverley Cemetery, a tablet adorns the grave of Lawrence O’Hara, a Member of the Legislative Assembly who died of influenza before he could take office. [6] The headstone of New Zealander William Menzies, who expired from the disease at North Head Quarantine Station on Armistice Day, is accompanied by a poignant footstone engraved ‘Daddy’.
The horse trough dedicated to Voluntary Aid Detachment worker Leela Prince, October 1933 [Image courtesy City of Sydney Archives, 020343]
Could it happen again?
In the century since 1918, medical scientists have established that the pandemic was caused by a particular strain of virus, influenza A H1N1. It was likely so infectious and severe because it was a new form that few people had immunity against. Where it came from, why it particularly affected younger adults and why it was so lethal continue to be debated. It seems likely that the deadly ‘pneumonic’ stage could have been due to bacteria entering the lungs following the virus infection, but it may also have triggered an over-active immune response. [11]
The impact of pneumonic influenza also continues to shape government, medical and cultural ideas about the power of highly infectious diseases. In recent decades the combination of annual vaccines against major influenza strains, plus effective antibiotic drugs, has greatly reduced the risk of a similar pandemic ever occurring again. [12]
Yet the ‘Spanish flu’ pandemic also created an enduring and intimate impact, remaining alive in personal memories, family stories and community legends. [13] In 2019 one informant related that, in 1919, her grandfather collapsed directly after reading her father a bedtime story. His death resulted in the loss of the family home, while her grandmother ‘had to go back to work as a nurse and … my father had to go to a boarding school’. [14] A century later, the hollow grief and bitterness of those days continues to resonate through intimate memories of this appalling pandemic.
References
An Unstoppable Enemy
[1] Peter Curson and Kevin McCracken, ‘An Australian Perspective of the 1918–19 Influenza Pandemic’, NSW Public Health Bulletin, Vol. 17, No. 7–8, 2006, p.103.
[2] Howard Phillips, ‘The Recent Wave of “Spanish” Flu Historiography’, Social History of Medicine, Vol. 27, No. 4, 2014, pp.796–7.
[3] Tom Quinn, Flu: A Social History of Influenza, New Holland Publishers, London, 2008, pp.125–6.
[4] Mark Honigsbaum, A History of the Great Influenza Pandemics: Death, Panic and Hysteria, 1830–1920, I. B. Tauris & Company, London, 2013, p.181.
[5] W.G. Armstrong, ‘Part I – Epidemiology and Administration’, in Report of the Director-General of Public Health, New South Wales, for the Year Ended 31st December, 1919, William Applegate Gullick, Sydney, 1920, pp.144–70.
[6] Clinical Notes on Pneumonic Influenza Epidemic, 1919, Melbourne: National Archives of Australia (hereafter NAA), Series MP367/1 Control 527/21/1077, H. Baret, [clinical notes on pneumonic influenza epidemic], 13 March 1919.
[7] Herbert French, ‘The Clinical Features of the Influenza Epidemic of 1918–19’, in Report on the Pandemic of Influenza, 1918–19, His Majesty’s Stationery Office, London, 1920, pp.66–109.
[8] Ibid., pp.73–5.
The Tide of Infection
[1] G. Dennis Shanks, et al., ‘Mortality Risk Factors during the 1918–1919 Influenza Pandemic in the Australian Army’, Journal of Infectious Diseases, Vol. 201, No. 12, 2010, pp.1880–9.
[2] J.H.L. Cumpston, Influenza and Maritime Quarantine in Australia, Albert J. Mullett, Melbourne, 1919, p.52.
[3] Spanish Influenza: Conference at Melbourne. Precautionary Measures, Canberra: NAA, A2 1919/482 PART 2, ‘Commonwealth and States of Australia. Influenza Conference 1918. Resolutions’, 27 November 1918.
[4] Anthea Hyslop, ‘A Question of Identity: J. H. L. Cumpston and Spanish Influenza, 1918–1919’, Australian Cultural History, Vol. 16, 1997, pp.60–76.
[5] Nick Wilson, et al., ‘Age-Specific Mortality during the 1918–19 Influenza Pandemic and Possible Relationship to the 1889–92 Influenza Pandemic’, Journal of Infectious Diseases, Vol. 210, No. 6, 2014, pp.993–5.
[6] ‘The Influenza Epidemic’, Sydney University Medical Journal, Vol. XIV, No. 1, 1919, pp.3–4.
[7] A. H. Brogan, Committed to Saving Lives: A History of the Commonwealth Serum Laboratories, Hyland House, South Yarra, 1990, pp.12–18.
[8] W.G. Armstrong, ‘Part I – Epidemiology and Administration’, in Report of the Director-General of Public Health, New South Wales, for the Year Ended 31st December, 1919, William Applegate Gullick, Sydney, 1920, pp.155, 162–4.
Influenza Comes Ashore
[1] G. Dennis, Shanks, Michael Waller, Alison MacKenzie and John F. Brundage, ‘Determinants of Mortality in Naval Units during the 1918–19 Influenza Pandemic’, Lancet Infectious Diseases, Vol. 11, No. 10, 2011, pp.793–9.
[2] Steven Bullard, In Their Time of Need: Australia’s Overseas Emergency Relief Operations 1918–2006, Cambridge University Press, Cambridge, 2017, pp.61–77.
[3] Ryan McLane, ‘Influenza and Quarantine in Samoa’, in Alison Bashford (ed.), Quarantine: Local & Global Histories, Palgrave, London, 2016, pp.136–53.
[4] Peter Curson, Deadly Encounters: How Infectious Disease Helped Shape Australia, Arena Books, Bury St Edmonds, 2015, pp.60–87.
[5] Patrick George Hodgson, ‘Flu, Society and the State: The Political, Social and Economic Implications of the 1918–1920 Influenza Pandemic in Queensland’, unpublished PhD thesis, James Cook University, 2017, pp.77–111.
[6] Jean Whitla, Memories 4 of Old Wodonga. Compiled for Wodonga Historical Society from Government Records and Reports, Newspapers, the Recollections of People and the Society’s Archive, Wodonga Historical Society, Wodonga, 2009, pp.78–85.
[7] J.H.L. Cumpston, Influenza and Maritime Quarantine in Australia, Albert J. Mullett, Melbourne, 1919, pp. 55–62.
[8] Peter Curson and Kevin McCracken, ‘An Australian Perspective of the 1918–19 Influenza Pandemic’, NSW Public Health Bulletin, Vol. 17, No. 7–8, 2006, pp.103–4.
[9] G. H. Knibbs, The Official Year Book for the Commonwealth of Australia, Containing Authoritative Statistics for the Period 1901–1919 and Corrected Statistics for the Period 1788 to 1900, Albert J. Mullett, Melbourne, 1920, pp.1129–32.
[10] David Noonan, Those We Forget: Recounting Australian Casualties of the First World War, Melbourne University Press, Carlton, 2014, chapter 6.
Into Homes and Hearts
[1] Jack Camm, ‘The “Spanish” Influenza Pandemic: Its Spread and Patterns of Mortality in New South Wales during 1919’, Australian Historical Geography, Vol. 6, 1984, pp.13–25.
[2] Kevin McCracken and Peter Curson, ‘Flu Downunder: A Demographic and Geographic Analysis of the 1919 Epidemic in Sydney, Australia’, in Howard Phillips and David Killingray (eds.), The Spanish Influenza Pandemic of 1918–19: New Perspectives, Routledge, London, 2003, pp.110–31.
[3] Peter Curson, Deadly Encounters: How Infectious Disease Helped Shape Australia, Arena Books, Bury St Edmonds, 2015, p.64.
[4] H.A. Smith, ‘Part II – Mortality Statistics’ in Report of the Director-General of Public Health, New South Wales, for the Year Ended 31st December, 1919, William Applegate Gullick, Sydney, 1920, p.173.
[5] Anna Weatherly, ‘The 1919 influenza epidemic’, Recollections, No. 3, 2017, pp.4–7.
[6] W.G. Armstrong, ‘Part I – Epidemiology and Administration’, in Report of the Director-General of Public Health, New South Wales, for the Year Ended 31st December, 1919, William Applegate Gullick, Sydney, 1920, pp.170.
[7] Roy Vescya Graham, ‘The Influenza Epidemic in North Eastern New South Wales in 1919’, unpublished MD thesis, Rare Books and Special Collections, University of Sydney, 1920, p.8.
[8] Ibid., p.9–10.
[9] Smith, ‘Part II’, p.180.
[10] Armstrong, ‘Part I’, p.144.
[11] C.S. Willis, Practical Australian Sanitation: A Reference Book for Municipal Councils, Stock-Owners, Architects and Sanitary Engineers, Vol. I., William Brooks & Company, Sydney, 1923, Preface.
[12] Armstrong, ‘Part I’, p.147.
[13] Camm, ‘The “Spanish” Influenza Pandemic’, pp.21–3.
[14] Gordon Briscoe, Queensland Aborigines and the Spanish Influenza Pandemic of 1918–1919, Aboriginal Studies Press, Canberra, 1996, pp.10–12.
[15] Ibid., p.13.
[16] Graham, ‘The Influenza Epidemic in North Eastern New South Wales in 1919’, p.4.
[17] Ibid.
Regulation and Mobilisation
[1] W.A. Holman, ‘To the People of New South Wales’, Sydney Morning Herald, 3 February 1919, p.5.
[2] Anthea Hyslop, ‘Old Ways, New Means: Fighting Spanish Influenza in Australia, 1918–1919’, in Linda Bryder and Derek A. Dow (eds.), New Countries and Old Medicine: Proceedings of an International Conference on the History of Medicine and Health, Auckland, New Zealand, 1994, Auckland University Press, Auckland, 1995, pp.54–60.
[3] Milton J. Lewis, ‘Public Health in Australia from the Nineteenth to the Twenty-First Century’, in Milton J. Lewis and Kerrie L. MacPherson (eds.), Public Health in Asia and the Pacific: Historical and Comparative Perspectives, Routledge, Abingdon, 2007, pp.224–8.
[4] Shirley Evans, The Influenza Pandemic of 1918–1919 in the Blue Mountains (and Lithgow), Springwood Historical Society, Springwood, 1998, pp.5–25.
[5] Pneumonic Influenza – Claims Committee, 1918–19, Sydney: State Archives & Records New South Wales (hereafter SARNSW), Series NRS 906 Folder 5/5348.1, H.C. McLean to E.B. Harkness, 19 February 1919.
[6] SARNSW, 906 5/5348.1, B Green to Mr Fitzgerald, 19 April 1919.
[7] SARNSW, 906 5/5348.1, Telegram to Green, c.20 April 1919.
[8] Kathleen Woodgate, ‘The Spanish Flu Epidemic’, in Voices from a Vanishing Australia: Recollections of the Way Things Used to Be, ABC Enterprises, Crows Nest, 1988, pp.44–7.
[9] Melanie Oppenheimer, Red Cross VAs: A History of the VAD Movement in New South Wales, Ohio Productions, Walcha, 1999, pp.45–52.
[10] ‘Obituary. Nurse Marion Robinson’, The Northern Champion, 16 July 1919, p.2.
Grief, Recovery and Memory
[1] Condolence letters, cards and telegrams sent to Sydney and Elizabeth Butler on the occasion of the death of their teenaged son, Keith, from Spanish influenza, 1919, Sydney: State Library of New South Wales, MLMSS 10131.
[2] Pauline Curby, ‘A Grim Shadow: The Influenza Pandemic’, History, No. 136, 2018, pp.15–17.
[3] Nick Wilson, et al., ‘Remembering the 1918 Influenza Pandemic: National Survey of Memorials and Scope for Enhancing Educational Value around Pandemic Preparedness’, New Zealand Medical Journal, Vol. 130, No. 1465, 2017, pp.53–70.
[4] Jeremy Youde, ‘Covering the Cough? Memory, Remembrance, and Influenza Amnesia’, Australian Journal of Politics & History, Vol. 63, No. 3, 2017, pp.357–68.
[5] ‘Dr John Brooke Moore & Dr Brooke Moore’, Monument Australia, <http://monumentaustralia.org.au/display/20239-dr-john-brooke-moore-and-dr-brooke-moore>, accessed 23 January 2019.
[6] Alderman L. J. O`Hara’, Monument Australia, <http://monumentaustralia.org.au/display/109078-alderman-l.-j.-o%60hara>, accessed 23 January 2019.
[7] ‘Nurse Ruby Dickinson’, Monument Australia, <http://monumentaustralia.org.au/display/23268-nurse-ruby-dickinson>, accessed 23 January 2019.
[8] Memorial horse trough for VAD Leela Prince, Circular Quay, Sydney, c.1934, Sydney: City of Sydney Archives, NSCA CRS 538/375.45–52.
[9] ‘Kate Burke’, Monument Australia, <http://monumentaustralia.org.au/display/95220-kate-burke>, accessed 23 January 2019.
[10] ‘Obituary. Miss Kate Burke’, Braidwood Review and District Advocate, 15 July 1919, p.2.
[11] Mark Honigsbaum, ‘Spanish Influenza Redux: Revisiting the Mother of All Pandemics’, Lancet, Vol. 391, No. 10139, 2018, pp.2492–5.
[12] Australian Government Department of Health, Australian Health Management Plan for Pandemic Influenza, Department of Health, Canberra, 2014, pp.20–3.
[13] Lucy Taksa, ‘The Masked Disease: Oral History, Memory and the Influenza Pandemic 1918–19’, in Kate Darian-Smith and Paula Hamilton (eds.), Memory and History in Twentieth-Century Australia, Oxford University Press, Melbourne, 1994, pp.77–91.
[14] Helen Roberts, response to Peter Hobbins, ‘100 years later, why don’t we commemorate the victims and heroes of ‘Spanish flu’?’, The Conversation, <https://theconversation.com/100-years-later-why-dont-we-commemorate-the-victims-and-heroes-of-spanish-flu-109885>, accessed 21 January 2019.
Author: Dr Peter Hobbins, RAHS Councillor
Images: Sourced by Dr Peter Hobbins, RAHS Councillor
Web design: Laura Signorelli, RAHS Digital Coordinator